The Future of Wound Care: How Medical Breathable Barrier Nonwoven Fabrics Are Changing Healthcare
2025-07-10
Understanding Medical Breathable Barrier Nonwoven Fabrics
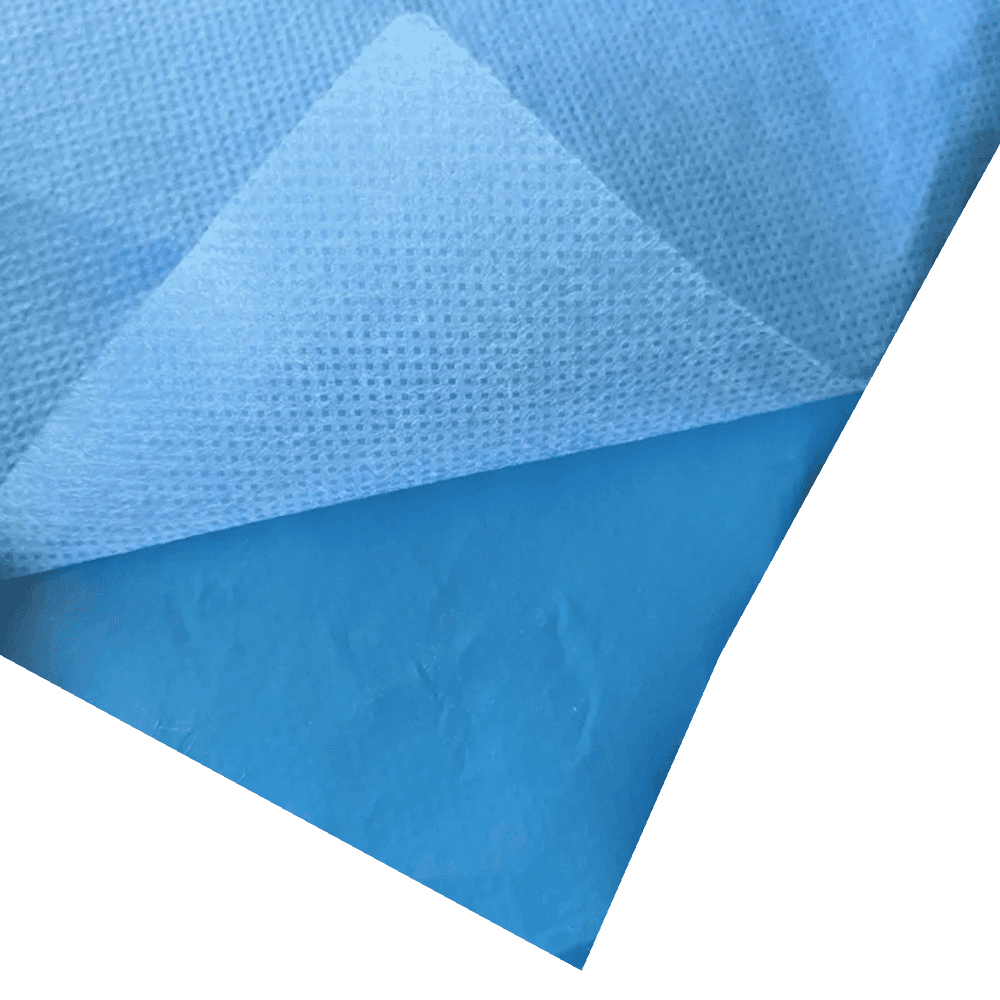
In modern healthcare, medical breathable barrier nonwoven fabric has emerged as a revolutionary material that combines protection with comfort. These advanced fabrics are engineered to allow air and moisture vapor to pass through while blocking liquids, bacteria, and other contaminants. Unlike traditional woven materials, nonwoven fabrics are produced by bonding or felting fibers together through mechanical, thermal, or chemical processes.
1.1 Key Characteristics of High-Quality Medical Nonwoven Fabrics
The effectiveness of medical-grade breathable nonwoven materials depends on several critical factors. First is breathability, measured by moisture vapor transmission rate (MVTR), which typically ranges between 2000-5000 g/m²/24hr for high-performance medical fabrics. Second is barrier performance, with most medical-grade materials achieving >99% bacterial filtration efficiency. Third is comfort, determined by factors like weight (usually 20-50 gsm for medical applications) and softness.
When comparing different types:
| Property | Standard Nonwoven | Medical Breathable Barrier |
|---|---|---|
| MVTR (g/m²/24hr) | 500-1500 | 3000-5000 |
| Bacterial Filtration | 90-95% | >99% |
| Liquid Strike-through | 3-10 seconds | >30 minutes |
| Weight (gsm) | 15-30 | 25-50 |
1.2 Manufacturing Processes for Medical Barrier Fabrics
The production of breathable nonwoven fabric for surgical drapes involves specialized techniques. Spunbond-meltblown-spunbond (SMS) is the most common, creating a three-layer structure that balances strength, barrier properties, and breathability. Other methods include hydroentanglement for softer fabrics and flash-spun for high-strength applications. Each method affects the final product's properties significantly.
Applications in Modern Medical Settings
The versatility of medical breathable barrier nonwoven fabric has led to its adoption across numerous healthcare applications. From surgical suites to outpatient clinics, these materials provide essential protection while maintaining patient comfort.
2.1 Surgical and Procedural Applications
In operating rooms, disposable medical nonwoven protective materials serve multiple critical functions. Surgical drapes made from these fabrics create sterile fields while allowing moisture vapor from the patient's body to escape. Compared to traditional reusable linen drapes, nonwoven alternatives reduce infection risks by 40-60% according to clinical studies. Surgical gowns benefit similarly, with modern versions offering better breathability than older plastic-coated alternatives.
2.2 Wound Care Innovations
Advanced wound dressings utilizing antimicrobial breathable nonwoven fabric represent one of the most significant improvements in chronic wound management. These dressings maintain optimal moisture balance (not too wet, not too dry) which clinical trials show can accelerate healing by 20-30% compared to traditional gauze. The three-dimensional structure of nonwoven fibers also helps prevent dressing adherence to wounds, reducing trauma during changes.
Technical Advantages Over Traditional Materials
The superiority of medical breathable barrier nonwoven fabric becomes evident when examining its technical specifications and performance metrics against conventional options.
3.1 Barrier Performance Comparison
Modern medical nonwovens achieve remarkable protection levels while maintaining breathability. For example, high-end surgical barrier fabrics can block blood penetration at pressures exceeding 100 mmHg while still allowing over 3000 g/m²/24hr of moisture vapor transmission. This combination was impossible with earlier materials that typically sacrificed one property for the other.
3.2 Comfort and Wearability Factors
Healthcare worker feedback consistently rates medical-grade breathable nonwoven materials higher than traditional options in comfort surveys. Key comfort metrics include:
| Comfort Factor | Nonwoven | Woven Cotton | Plastic-Coated |
|---|---|---|---|
| Air Permeability (cfm) | 10-20 | 30-50 | 0-5 |
| Surface Temperature Increase (°C) | 1.5-2.5 | 1.0-1.5 | 4.0-6.0 |
| Moisture Accumulation (g/m²/hr) | 5-10 | 15-25 | 30-50 |
Environmental Considerations and Sustainability
While medical breathable barrier nonwoven fabric offers numerous clinical advantages, its environmental impact requires careful consideration and ongoing innovation.
4.1 Disposable vs Reusable Debate
The healthcare industry continues to evaluate the balance between infection control and environmental sustainability. Life cycle assessments show that while disposable medical nonwoven protective materials generate more immediate waste, they often have lower total environmental impact than reusable alternatives when considering water, energy, and chemical use in laundering. New biodegradable nonwoven materials are emerging to address these concerns.
4.2 Recycling Challenges and Solutions
Standard medical-grade breathable nonwoven materials present recycling difficulties due to potential contamination and material complexity. However, recent developments include mono-material constructions that are easier to recycle and plant-based polymers that compost under industrial conditions. These innovations aim to maintain performance while reducing environmental footprint.
Future Directions in Medical Nonwoven Technology
The evolution of medical breathable barrier nonwoven fabric continues at a rapid pace, driven by both clinical needs and technological advancements.
5.1 Smart and Responsive Materials
Next-generation antimicrobial breathable nonwoven fabric incorporates responsive elements that change properties based on environmental conditions. Examples include fabrics that increase breathability when moisture levels rise or release antimicrobial agents only when bacteria are detected. These innovations could revolutionize infection control in healthcare settings.
5.2 Enhanced Performance Through Nanotechnology
Nanofiber-based nonwovens are pushing the boundaries of what breathable nonwoven fabric for surgical drapes can achieve. With fiber diameters measured in nanometers rather than micrometers, these materials offer superior barrier properties at lower weights, improving both protection and comfort. Early studies suggest nanofiber drapes may reduce surgical site infections by an additional 15-20% compared to standard SMS materials.


 日本語
日本語 Русский
Русский España
España عرب .
عرب .